Sonntag, Oktober 31, 2010
Back Pain and its Management: Myths and Misconceptions
Samstag, Oktober 30, 2010
Botox for Migraine
发自我的 iPhone
欧洲也才批准了Botox注射治疗偏头痛。
十分可笑的是注射部位,那不是对传统的偏头痛理论的颠覆?
是的,应该颠覆。
以我在德国5年的治疗方法,这个注射也是要被颠覆的。
因为,我从来就是在后方治疗,而80%的患者前额和眼部的症状消失。那些症状无非是一些牵涉痛,反射痛罢了。
Botox for Migraine
Over the past few years, there has been increased interest in using Botox for migraine. Some people feel it has been an almost miraculous solution for them. But the trials and research hasn't always been convincing. Is Botox for migraines something you should try?
A little background on Botox
Botox is botulinum toxin, a toxin produced by bacteria. It's actually extremely poisonous, and often is ingested as a result of not handling and cooking meat properly (botulism is often fatal).
But botulinum toxin A (Botox) has become famous for it's other application - getting rid of wrinkles. The treatment was discovered in Canada in 1987 by Jean and Alastair Carruthers, and since then brand names Botox, Neurobloc and Myobloc (botulinum toxin B) have been used (in very small doses) to decrease wrinkles and frown lines.
But the next discovery was that patients with migraine found their attacks to be decreasing when they had Botox treatment. Why was this happening? Was it just a coincidence?
Since then, research has begun to try to understand why it works, and when it works, and how Botox for migraine might best be used.
How does it work?
In your body, a chemical (neurotransmitter) known as acetylcholine sends signals for muscles to contract. Botox as a toxin binds the nerve endings, blocking the release of the chemical. Essentially, your muscles don't get the message to contract, and so they relax. In a proper treatment, the muscles won't contract (causing wrinkles), but will still have enough strength for normal use.
Why it may work to relieve migraine is not certain. Could it just be that relaxing certain muscles slows the migraine chain reaction? It's more likely that it blocks pain signals, or may even block signals that contribute to the migraine.
An article at the Mayo Clinic simply says,"the drug may cause changes in your nervous system that modify your tendency to develop migraines".
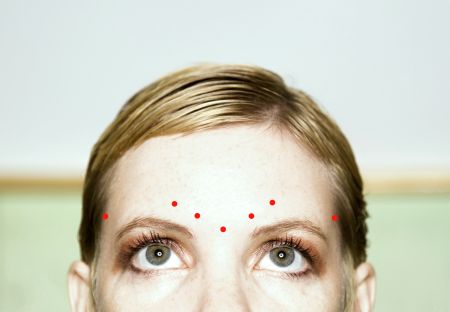
Botox injected in the forehead for migraines
Botox for migraine - injections
So just how is Botox for migraines used? Well, one way is through simple injections. The treatment is given in a series of shots. Some patients have found almost immediate relief. But the interesting thing is that the improvement tends to last for several months.
The injections may be expensive. Many patients need to weigh the cost against the amount of improvement they receive and the length of time the injections seem to help for. It's important to discuss the option with your doctor and keep a headache diary.
Neither are all injections created equal. Sometimes injections are simply done in a band-like fashion around the skull. But as our understanding increases about what works, different approaches, more specific approaches are being taken.
For example, Dr Jeffrey E. Janis advocates finding "peripheral trigger points", using them as a roadmap to use Botox for migraine.
Read more here about what Botox headache injections are like.
Botox and surgery
Dr. Janis' believes that this process can go even farther. The newer idea is that the Botox injections can find those trigger points - and then surgery can do the rest.
Instead of using a shotgun approach - simply injecting everyone the same way - some researchers believe that you can use the injections as a test. Which muscles are triggering the migraine attacks? If those specific muscles can be found, surgery can keep the problem from resurfacing in the future.
Dr Janis explains: "It's like a math equation. I will inject the Botox into one trigger point at a time and leave the others alone. The Botox is used as a diagnostic test to determine what trigger point is causing the problem. If patients get a benefit from the Botox, they likely will get a benefit from the surgery. If there's no benefit from the Botox, then there won't be a benefit from the surgery."
This treatment has some very controversial aspects. Of course, most are sceptical that migraine can be relieved by focusing on muscles. Though muscle problems may be a trigger, it's generally accepted that the migraine problem itself lies deep in the brain. Muscle issues may actually be a trigger in only a few migraine sufferers.
Still not ready for prime-time?
Groups like the American Academy of Neurology are not ready to accept Botox for migraine as a major treatment. In the spring of 2008, they suggested that Botox injections were no better than a placebo, based on the current evidence. (Read Botox Works on Muscle Disorders But Not Migraines) They recommended that this treatment not be suggested for people with episodic migraine and chronic tension-type headaches.
But wait - what about all these people that claim Botox has changed their lives, by relieving migraine? Well, the fact of the matter is that the research is still in its infancy. It seems that Botox treatments do work, for some. And for some they work very well.
But when compared against the many other treatments out there, the evidence still needs to be built up. In other words, there are many other things you can try, and probably should try, before you try Botox for migraine.
Some research is starting to suggest that patients with certain kinds of migraine pain may benefit most from Botox. That would explain why the more general studies don't show the same improvements. (Read this study on exploding vs imploding headache, for example, from 2007)
And different studies measure things differently. For example, what if Botox for migraines decreased the frequency of migraine attacks, but not the intensity?
If you are interested in trying Botox, take a look at some of the latest techniques, and discuss them with your doctor. Be sure you have a good idea what else is out there, and what the pros and cons are.
Read more about some of the earlier Botox for migraine studies here.
Freitag, Oktober 29, 2010
太极武当 / 有形无形 /德国科隆的设计师
居然要请德国科隆人为武当山设计建筑,看来我家乡的人越来越有国际大视野了。那个德国老先生竟然了解老子,年轻时有一本老子的口袋书,还带上战场。
节目最后,那个领导,似乎以前在茅箭区工作过吧。
Neues Gesicht, neues Leben, 新生活需要新面孔,看到他我很吃惊。
Dallas Wiens Gesicht war durch einen Arbeitsunfall bis zur Unkenntlichkeit entstellt worden. Eine komplizierte Operation soll dem Amerikaner bald ein ein neues Antlitz schenken.
Er verfügt weder über Augen noch über eine Nase. An der Stelle, bei der in einem Gesicht der Mund zu finden ist, zeigt sich lediglich ein Schlitz ohne Lippen.
Dallas C. Wiens war ein ganz normaler Twen, bis sich sein Leben durch einen Unfall während der Ausübung seines Jobs drastisch veränderte: Er geriet an eine Hochspannungsleitung, die sein Gesicht vollständig verbrannte. Seither musste der 25-jährige Vater einer kleinen Tochter mehrere Hauttransplantationen über sich ergehen lassen - klassische Gesichtsmerkmale konnten dabei nicht wiederhergestellt werden, bisher: Dallas Wiens bekommt bald ein neues Aussehen - ihm wird ein komplettes Gesicht verpflanzt. (dga/rre)
<img src="http://20min.wemfbox.ch/cgi-bin/ivw/CP/iApp/iphoneapp/feed" width="1" height="1" border="0" />
<img src="http://20minde.wemfbox.ch/cgi-bin/ivw/CP/iApp/iphoneapp/feed" width="1" height="1" border="0" />
Von meinem iPhone gesendet
Donnerstag, Oktober 28, 2010
Montag, Oktober 25, 2010
Sonntag, Oktober 24, 2010
New treatments for Dupuytren contracture 注射用XIAFLEX(collagenase clostridium histolyticum)溶组织芽胞胶原酵素
发自我的 iPhone
我观察Dr.Eaton两年多了。也许有一天会在美国见到他。
D. Kay Kirkpatrick, MD | Roy A. Meals, MD |
F. Thomas D. Kaplan, MD | Charles Eaton, MD, FACS |
October 2010 Issue
http://www.aaos.org/news/aaosnow/oct10/clinical2.asp
Samstag, Oktober 23, 2010
Sonntag, Oktober 17, 2010
Samstag, Oktober 16, 2010
Freitag, Oktober 15, 2010
Mittwoch, Oktober 13, 2010
"观于海者难为水,游于圣人之门者难为言"
那些家庭医生不是一般的难对付。
介绍了两个病人,
一个是腰椎手术后综合症,我们治疗后不用服鸦片类止痛药了,随访了4年。
一个是紧张性头痛的患者,今年3月治疗,5年的头痛,一次治疗,不再复发。随访了7个月。
发自我的 iPhone
Dienstag, Oktober 12, 2010
FOCUS Online: Eine Schachtel kostet bis zu 107 Euro
Rauchen - Eine Schachtel kostet bis zu 107 Euro
http://tinyurl.com/363df9x/?mobile=no
Von meinem iPhone gesendet
Montag, Oktober 11, 2010
Freitag, Oktober 08, 2010
FOCUS Online: Elektrische Entladungen im Gehirn
Epilepsie - Elektrische Entladungen im Gehirn
http://tinyurl.com/247qlx5/?mobile=no
Von meinem iPhone gesendet
Donnerstag, Oktober 07, 2010
stern.de: Kinderkrankheit Rückenschmerzen
Krankenkassen-Studie - Kinderkrankheit Rückenschmerzen
Link zum AppStore: http://itunes.apple.com/de/app/stern-de/id306192028?mt=8
Von meinem iPhone gesendet
Dienstag, Oktober 05, 2010
stern.de: Die Kleinen besiegen die Großen 电子阅读器比较
E-Book-Reader im Test - Die Kleinen besiegen die Großen
Link zum AppStore: http://itunes.apple.com/de/app/stern-de/id306192028?mt=8
Von meinem iPhone gesendet
Sonntag, Oktober 03, 2010
stern.de: Die verwirrende Vielfalt der App-Stores
Smartphone-Helferlein - Die verwirrende Vielfalt der App-Stores
Link zum AppStore: http://itunes.apple.com/de/app/stern-de/id306192028?mt=8
Von meinem iPhone gesendet
Samstag, Oktober 02, 2010
明天德国重新统一20年
20年庆典前,今年在不来梅,中国确实不应该一直在北京
三个城市
20年前后对照
2010.10.3
Der Islam gehört zu Deutschland,总统讲话
BERLIN - DAMALS UND HEUTE,柏林今昔
Prager Botschaft,前西德住捷克大使馆,除柏林墙,这里也值得纪念
Deutschland-von-A-bis-Z
Der Tag der Deutschen Einheit,历史时刻
Freitag, Oktober 01, 2010
Blog-Archiv
-
▼
2010
(240)
-
▼
Oktober
(36)
- Back Pain and its Management: Myths and Misconcept...
- Botox for Migraine
- 太极武当 / 有形无形 /德国科隆的设计师
- Deutsches Ärzteblatt: Archiv "Arthrose: Kein alter...
- Neues Gesicht, neues Leben, 新生活需要新面孔,看到他我很吃惊。
- Nearly 1 Million Fentanyl Pain Patches Recalled
- 【面对面】2010.10.24 — 印象·张艺谋
- New treatments for Dupuytren contracture 注射用XIAFLE...
- Treating spinal compression fractures
- Long-Term Use of Corticosteroid Injections for Ten...
- Wochenmarkt
- 63 Ways to Build Self-Confidence and Self-Esteem |...
- Osteoporose: Unentdeckte Frakturen - News - FOCUS ...
- Botox Approved for Headache Prophylaxis in Chronic...
- 20 Minuten Online - Ein Tag für die Geschichtsbüch...
- Neuroscientists say love really is like a drug - H...
- "观于海者难为水,游于圣人之门者难为言"
- FOCUS Online: Eine Schachtel kostet bis zu 107 Euro
- New technologies and surgical techniques promise '...
- SPIEGEL MOBIL: Friedensnobelpreis für Pekings Staa...
- FOCUS Online: Elektrische Entladungen im Gehirn
- stern.de: Kinderkrankheit Rückenschmerzen
- Nobelprize.org
- left arm pain
- Secret Left Arm Pain Information Finally Revealed ...
- Österreich Journal
- gesundheit medizin - oneJournal - Pressemitteilung...
- Dauerthema Migräne: Auslöser vermeiden ist falsch ...
- stern.de: Die Kleinen besiegen die Großen 电子阅读器比较
- stern.de: Die verwirrende Vielfalt der App-Stores
- 20 Jahre deutsche Einheit: 3. Oktober: Live-Blog, ...
- AUERGLASS
- 明天德国重新统一20年
- 嫦娥二号探月卫星发射现场直播
- 影像的力量:改变了当今世界的十张伟大摄影作品 - 超级苹果网新闻
- 我们的传统就是,敢于恶鬼争天下,不向霸王让寸分
-
▼
Oktober
(36)
Über mich

- H Chen
- In pain there is no east and west.I did it my way beyond them.